Antimicrobial Resistance: What is it and Why is it so Important?
FAASTsheet 01 /
What Are Antimicrobials?
Antimicrobials are drugs that kill or slow the growth of microorganisms (such as bacteria, fungi, parasites, and viruses). The term ‘antimicrobials’ is most commonly used to refer to antibiotics, which are used against bacteria, but this term also applies to antivirals, antifungals and antiparasitics.
Antimicrobials have helped satisfy a growing demand for animal protein by improving the efficiency of livestock and poultry production. Antimicrobials are important tools for farmers when it comes to preventing and treating illness in their animals.
What is Antimicrobial Resistance?
The widespread use of these drugs in humans and animals has led to antimicrobial resistance, which limits or removes our ability to treat human and animal illnesses with the drugs we are used to using.
Antimicrobial resistance (AMR) refers to microorganisms (such as bacteria) having the ability to survive even when drugs designed to kill them or limit their growth are present.
AMR can spread – The resistant microorganisms that survive in the presence of antimicrobials continue to multiply, creating whole populations of resistant microorganisms. Bacteria can also spread their resistance to other species of bacteria by sharing small pieces of their DNA.
Why is AMR Important?
It’s estimated that over 2 million human illnesses are caused by AMR infections in the USA each year, resulting in approximately 23,000 deaths2. Globally, it is estimated that 700,000 die from AMR infections each year3.
If AMR continues to spread unchecked, by 2050 approximately 10 million people could die from AMR infections every year3 (Figure 1).
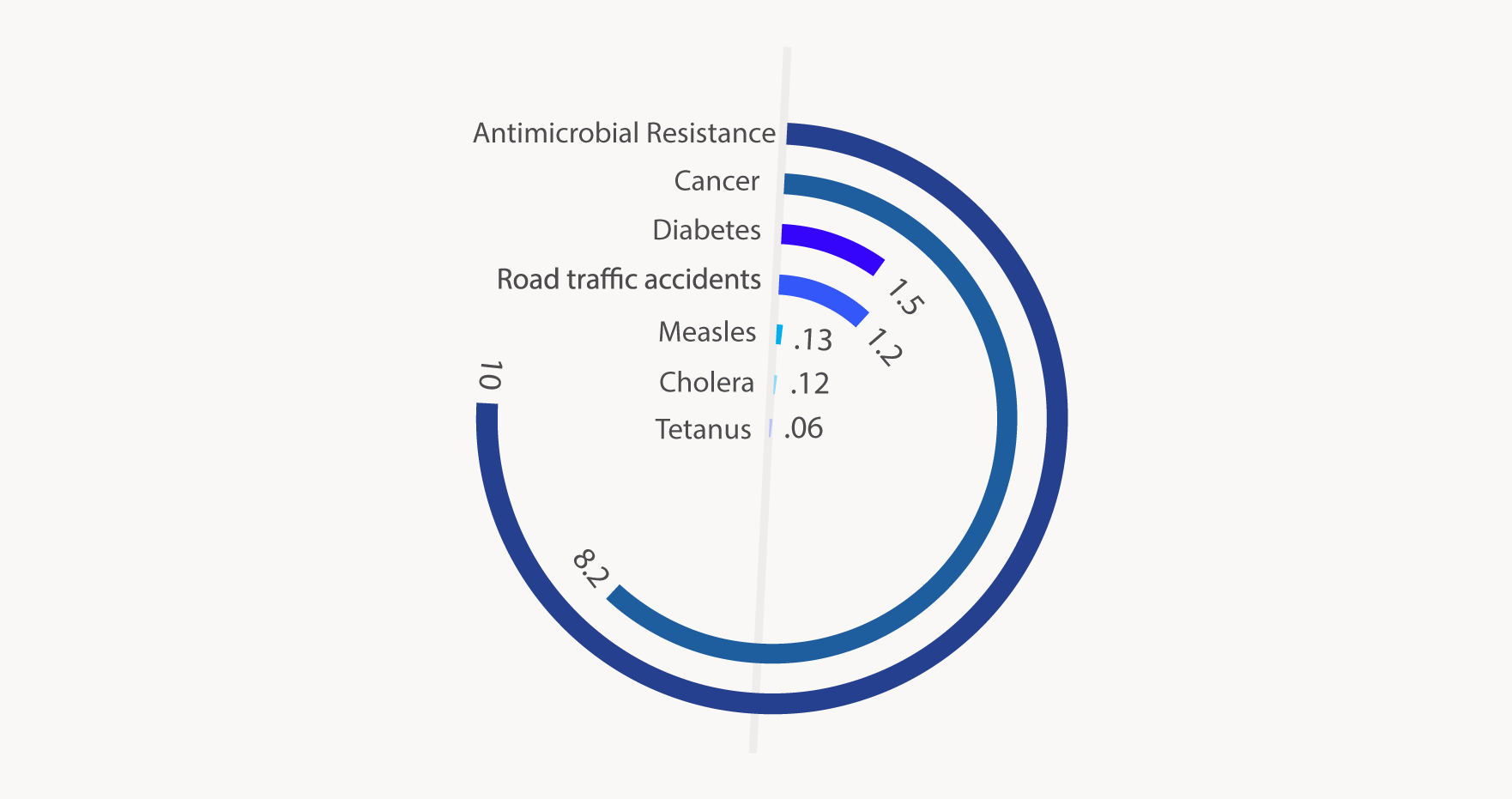)
Figure 1. Projected number of deaths due to antimicrobial resistance and other causes in 20503
Why Should I be Concerned About AMR?
- Animal health: An increase in resistant microorganisms means infections in animals become harder (or impossible) to treat, which leads to increased animal illness and death.
- Human health: Resistance in animals can spread to humans and lead to infections in people that are harder (or impossible) to treat. They spread from animals to humans by:
- Direct contact between farm workers and animals4;
- Contamination of foods of animal origin (e.g. meat, milk, eggs)5;
- Contamination of the environment with animal manure (e.g. runoff, fertilizer)6.
There is clear evidence that antimicrobial use (AMU) in animals plays a role in the development of AMR in humans4. Therefore, it is of utmost importance that we take action to minimize the development of AMR in animal populations.
Everyone who uses or prescribes antimicrobials has a role to play in fighting the spread of AMR
)
Preserving the Efficacy of Antimicrobials
The Public Health Agency of Canada has developed a strategy, “Tackling Antimicrobial Resistance and Antimicrobial Use: A Pan-Canadian Framework for Action”, to address AMR in human and animal populations. This framework focuses on:
-
Surveillance
Tracking AMR and AMU in humans and animals in Canada
-
Infection prevention and control
Communication on how to prevent and control illness, such as the use of biosecurity practices in livestock, which reduces the need to use antimicrobials in the first place
-
Antimicrobial stewardship
Designing programs focusing on education, awareness, and regulatory oversight to reduce inappropriate prescribing and dispensing of antimicrobials in humans and animals, and to promote other means of maintaining health and preventing infections
-
Research
To better understand the development of AMR and develop new antimicrobials and alternatives to fight and prevent infections
Important Definitions
Antimicrobials – those natural or synthetic compounds that kill microorganisms (i.e. bacteria, fungi, parasites, viruses) or slow their growth.
Antibiotics – Antimicrobials that have activity against bacteria
Antimicrobial Stewardship – the multifaceted approaches required to sustain the efficacy of antimicrobials and minimize the emergence of AMR.9
Antimicrobial Use (AMU) – the employment of antimicrobial agents to kill or slow the growth of microorganisms
Antimicrobial Resistance (AMR) – the multifactorial process by which microorganisms (bacteria, fungi, parasites, viruses) naturally have, develop or acquire elements that enable them to survive in the presence of those antimicrobials (antibiotics, antifungals, anthelmintics, antivirals) designed to kill them or slow their growth.
One Health Approach – This approach to public health problems recognizes that the health of humans, animals, and the environment are deeply interconnected. Any health problem spanning the human-animal-environment interface necessitates a coordinated, collaborative, multidisciplinary and cross-sectoral approach to realize an effective solution.
For More Information
Videos
AMR in North America
- Centers for Disease Control: Antibiotic Resistance Threats in the United States, 2013
- Canadian Integrated Program for Antimicrobial Resistance Surveillance (CIPARS)
- Canadian Antimicrobial Resistance Surveillance System
Canada’s Response to the AMR Crisis
References
- Public Health Agency of Canada. Tackling Antimicrobial Resistance and Antimicrobial Use A Pan-Canadian.; 2017.
- CDC. Antibiotic resistance threats in the United States, 2013. CDC Rep. 2013.
- O’Neill J. Tackling drug-resistant infections globally: final report and recommendations. Rev Antimicrob Resist. 2016;(May):84. doi:10.1016/j.jpha.2015.11.005.
- Tang KL, Caffrey NP, Nóbrega DB, et al. Restricting the use of antibiotics in food-producing animals and its associations with antibiotic resistance in food-producing animals and human beings: a systematic review and meta-analysis. Lancet Planet Heal. 2017;1(8):e316-e327. doi:10.1016/S2542-5196(17)30141-9.
- PHAC. Canadian Integrated Program for Antimicrobial Resistance Surveillance (CIPARS) Annual Report – Antimicrobial Resistance. Public Health Agency Canada, Guelph, Ontario. 2014.
- Chang Q, Wang W, Regev-Yochay G, Lipsitch M, Hanage WP. Antibiotics in agriculture and the risk to human health: how worried should we be? Evol Appl. 2014:n/a-n/a. doi:10.1111/eva.12185.
- Holmes AH, Moore LSP, Sundsfjord A, et al. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet. 2016;387(10014):176-187. doi:10.1016/S0140-6736(15)00473-0.
- Page S, Prescott J, Weese S. Antimicrobial resistance: The 5Rs approach to antimicrobial stewardship. Vet Rec. 2014;175(8):207-208. doi:10.1136/vr.g5327.
- Giguere S, Prescott, JF, and Dowling, PM. Antimicrobial therapy in veterinary medicine. 2013. Fifth edition, Wiley Blackwell. Ames, Iowa, U.S.A. pp. 118.